ABOUT THE SPEAC PROJECT
The Coalition for Epidemic Preparedness Innovations (CEPI) is a global partnership that develops vaccines to stop future epidemics. Brighton Collaboration is an international community of vaccine safety experts that provides standardized, validated, and objective methods for monitoring vaccine safety profiles and benefit-risk ratios.
In 2019, CEPI and Brighton Collaboration came together to launch the Safety Platform for Emergency Vaccines (SPEAC), a CEPI-funded project. SPEAC aims to enhance safety for CEPI-funded trials across multiple platforms for multiple priority pathogens, including vaccines for Lassa fever, Nipah virus, MERS, and Chikungunya.
In 2022, CEPI announced its 100 Days Mission to dramatically reduce the time it takes to deliver a vaccine against a pandemic pathogen. New priorities were added to SPEAC’s work to support CEPI in achieving this ambitious goal, including a focus on outreach to low- and middle-income countries and facilitation of rapid response.
Mission
Objectives

SPEAC provides tools and services for harmonized safety monitoring in vaccine studies of known epidemic and pandemic threats by supporting all stakeholders involved in vaccine safety monitoring.
SPEAC harnesses the learnings around safety monitoring of vaccines to improve the efficiency of safety data collection and knowledge sharing.

Through the Brighton Collaboration and CEPI network SPEAC connects vaccine safety experts and stakeholders on a global scale.
SPEAC activities
Data Safety Monitoring Boards (DSMBs) for vaccines are typically composed of target disease experts, statisticians, and infectious disease specialists. Unfortunately, vaccine safety expertise is frequently missing.
SPEAC aims to contribute to that gap through DSMB support for vaccine developers and what SPEAC calls the Meta-DSMB:
DSMB Support for vaccine developers
SPEAC has created a pool of eligible candidates for DSMBs who are now available to CEPI-funded developers conducting trials in Africa and SE Asia contributing to the Research Preparedness Network initiative included in CEPI 2.0 plans for Clinical Development.
The pool has been continuously expanded through a training course conducted in priority geographic regions as one of the tasks within the SPEAC project.
Meta-DSMB
The meta-DSMB is a group of experts that monitors the safety profile of vaccines across all CEPI-funded clinical awardees by looking at patterns possibly related to vaccine platforms, antigens, adjuvants across trials.
The group comprises 16 global liaison members that attend the different awardees’ DSMBs as non-voting observers. They provide input on request and review reasons to stop/pause the enrolment of individual trials based on safety data and assess impact for similar vaccines/vectors.
A key task of the SPEAC project has been and continues to be the identification of ‘potential’ Adverse Events of Special Interest (AESI) that could occur during vaccine development of the he CEPI prioritized pathogens including Lassa Fever, MERS, Rift Valley Fever, Nipah, Chikungunya, COVID-19. These AESIs were identified based on based on vaccine safety evidence and target disease pathogenesis and the main objective is to
Once the AESIs have been identified, the work of the Standards and Tools work package in SPEAC focuses on ensuring the availability of the related resources below:
- Brighton Collaboration case definitions
- Risk factors for AESI occurrence to guide investigation & causality assessment
- Population based background incidence of AESI to facilitate ‘expected’ vs ‘observed’ signal assessments
- Medical codes (ICD, MedDRA, SNOMeD) to enable database searches for an AESI
- Case report forms and algorithms to assist uniform application of available data to apply the case definition
The main goal of the above process that harmonized lists of prioritized AESIs together with their related standardized case definitions, resources and tools are available for global use across the vaccine life cycle, especially in the context of pandemics and/or outbreaks.
Effective communication of key information among key stakeholders including regulators, public health, and the general public is challenging due to highly subspecialized research with many acronyms, and the lack of specialized training in data supporting vaccine safety by many key stakeholders. That ends app leading to delays in regulatory approval and diminished public acceptance.
In that context SPEAC started to develop standardized templates with key benefit/risk assessment considerations.
Templates can function as a checklist for risk management of complicated activities and might help prioritize future research despite the inevitable gaps in current data. They can facilitate provision of key benefit/risk data for policymakers and for regulators to support the decisions for early authorization in case of emergency use.
Digital Transformation (DT) is an industry best practice to advance vaccine discovery, clinical trials, regulatory approval, market distribution, and safety monitoring. Effective DT results in modernization of technology platforms and emergence of science-based informatics tools for vaccine developers.
In the context of SPEAC the project, one of the objectives is to create a SPEAC Safety Services Portal to accelerates the distribution and adoption of SPEAC best practice products and services to stakeholders.
The team will also focus on building data-driven connections between SPEAC products to facilitate collaboration as well as synergy around development and deployment of products by SPEAC; and for distribution of products to partners.
There is a need for better understanding of the unique aspects of special populations in the life cycle of vaccines for emergent and epidemic/pandemic infectious diseases, as well as for the timely assessment of special populations’ disease burden to assess their risk in the early phases of a new disease emergence and for prompt inclusion of special populations in vaccine research and implementation as opposed to exclusion from early research, and late implementation
The SPEAC project team activities related to special populations include:
- Identifying any special populations of relevance for the CEPI prioritized pathogens, and the workstreams of experts for each of the identified special populations.
- Ensuring the inclusion of special populations in the process of vaccine development, evaluation, and implementation to contribute to CEPI’s objectives.
- Supporting key stakeholders throughout the process of vaccine development, evaluation, and implementation for special populations. Tools will be developed and made accessible to facilitate the timely inclusion of special populations in the development, evaluation, and implementation of vaccines for selected emerging pathogens.
- Facilitating the interaction and integration of goals set up by SPEAC by providing special population level expertise.
The objective of this work package is to contribute to strategies for the generation of evidence of safety at CEPI Research Preparedness, as well as to strengthen the sustainability of such activities as it is critical for ongoing benefit-risk evaluation.
The fulfil its objective the main tasks of this SPEAC work package will focus on:
- Planning for rapid landscape assessment that profiles the current state of current and planned active surveillance in LMICs identified by CEPI Research Preparedness Network sites, including identification of critical gaps and obstacles to sustainability.
- Defining the requirements and the assessment of the capacity of these Network sites for active safety surveillance of vaccines.
- Integrating the CEPI Research Preparedness Network sites into existing networks of vaccine safety, promoting coordination and leveraging the efforts of others.
In the updated WHO R&D Blueprint list of priority diseases in February 2018, “Disease X” was included. “Disease X” is a term used to describe the possibility of a severe global epidemic caused by a pathogen that is not currently known to cause human disease and due to its unpredictable nature it is difficult to anticipate where it is likely to emerge or what it may be.
However, new diseases frequently arise from various parts of the world, particularly in developing countries with high levels of biodiversity. Such countries are at a greater risk of outbreaks due to their limited capacity for surveillance and response. COVID-19 is an example of “Disease X,” and as it has demonstrated, diseases do not respect borders. To respond to future outbreaks effectively, we must be prepared on a global scale.
SPEAC has funds that enable timely acute response to emergency vaccine safety issues; either during the development of candidate vaccine(s) against a new Disease X, or during the rollout of such new vaccines to larger populations when new AESI X might first emerge.
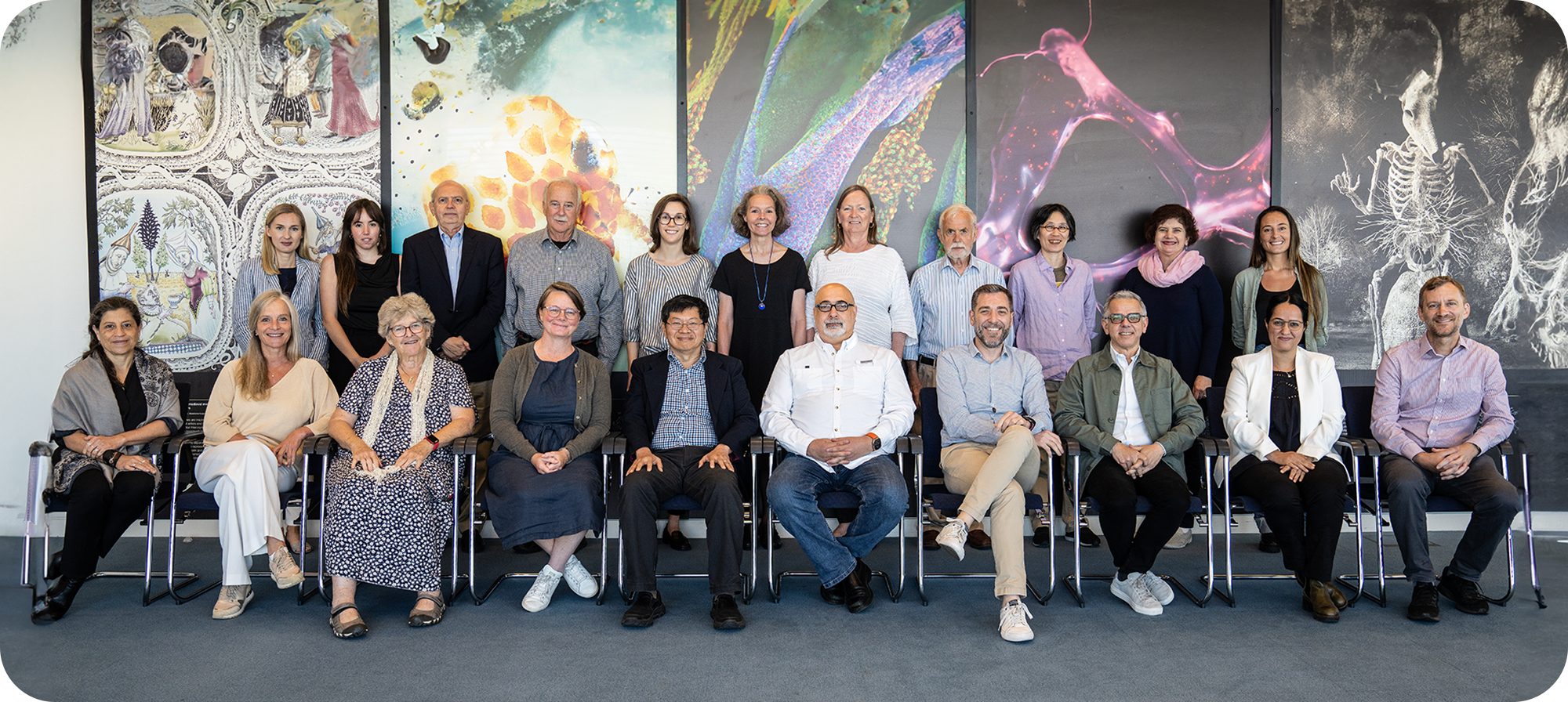
OUR TEAM
MANAGEMENT TEAM
Task Force For Global Health (Program Management)
WeDo (Project Management)
CEPI Members
BOARD
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Nulla suscipit, turpis ac posuere aliquet, mauris turpis congue arcu, eget porta justo massa ac felis.
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Nulla suscipit, turpis ac posuere aliquet, mauris turpis congue arcu, eget porta justo massa ac felis. Lorem ipsum dolor sit amet, consectetur adipiscing elit. Nulla suscipit, turpis ac posuere aliquet, mauris turpis congue arcu, eget porta justo massa ac felis.
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Nulla suscipit, turpis ac posuere aliquet, mauris turpis congue arcu, eget porta justo massa ac felis.
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Nulla suscipit, turpis ac posuere aliquet, mauris turpis congue arcu, eget porta justo massa ac felis.
INVESTORS & PARTNERS
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Nulla suscipit, turpis ac posuere aliquet, mauris turpis congue arcu, eget porta justo massa ac felis.
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Nulla suscipit, turpis ac posuere aliquet, mauris turpis congue arcu, eget porta justo massa ac felis. Lorem ipsum dolor sit amet, consectetur adipiscing elit. Nulla suscipit, turpis ac posuere aliquet, mauris turpis congue arcu, eget porta justo massa ac felis.
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Nulla suscipit, turpis ac posuere aliquet, mauris turpis congue arcu, eget porta justo massa ac felis.
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Nulla suscipit, turpis ac posuere aliquet, mauris turpis congue arcu, eget porta justo massa ac felis.
Project Partners